A single treatment of an investigational CRISPR/Cas9-based cell therapy could provide durable disease control for nearly all patients with transfusion-dependent beta-thalassemia and sickle cell disease.
After one infusion of exagamglogene autotemcel (exa-cell), 95% of patients with beta-thalassemia no longer required red blood cell transfusions and no patients with sickle cell disease experienced severe vaso-occlusive crises.
"These results indicate that exa-cell has the potential to be the first CRISPR/Cas9-based therapy to provide a one-time functional cure for beta-thalassemia and severe sickle cell disease," said first author Franco Locatelli, MD, a professor of pediatrics at the Sapienza University of Rome, Italy, and director of the Department of Pediatric Hematology and Oncology at Bambino Gesù Children’s Hospital, Rome, Italy.
Locatelli presented the late-breaking results on June 12 at the 2022 European Hematology Association (EHA) Annual Meeting in Vienna.
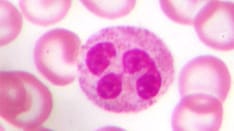
Transfusion-dependent beta-thalassemia and sickle cell disease share a distinct mutation in the hemoglobin beta subunit gene. This mutation reduces or eliminates the production of beta chains of hemoglobin or leads to abnormal hemoglobin polymerization upon deoxygenation.
Recently approved therapies, such as luspatercept and crizanlizumab, can improve symptoms, but are not curative. Allogeneic bone marrow transplantation represents a curative option, but compatible donors remain limited.
Exa-cell therapy approaches beta-thalassemia and sickle cell disease from another angle — it targets mechanisms that boost production of fetal hemoglobin, which is associated with improvements in both diseases. More specifically, the exa-cell therapy uses CRISPR/Cas9 to edit single-nucleotide polymorphisms in the BCL11A locus within autologous hematopoietic stem and progenitor cells, which can increase expression of fetal hemoglobin and reduce disease severity.
Previous data from pivotal trials CLIMB THAL-111 and CLIMB SCD-121 revealed that a single dose of exa-cell, formerly known as CTX001, can increase fetal hemoglobin and total hemoglobin enough to eliminate red blood cell transfusions and vaso-occlusive crises. The current investigation reported efficacy and safety data in the first 75 patients in these ongoing pivotal trials.
The 44 patients with beta-thalassemia and 31 with sickle cell disease underwent myeloablation with busulfan followed by a single exa-cell infusion.
Overall, 95% of patients with beta-thalassemia (42 of 44) no longer required red blood cell transfusions over the year follow-up. Even the two patients who did reduced their requirement by as much as 89%.
None of the 31 patients with sickle cell disease experienced severe vaso-occlusive crises.
Clinically meaningful increases in fetal hemoglobin and total hemoglobin levels were observed in both disease groups, with the increases maintained throughout the follow-up period.
Adverse events were consistent with those observed with myeloablative conditioning with busulfan and autologous stem cell transplant. Two patients with transfusion-dependent beta-thalassemia experienced serious adverse events considered related to exa-cell.
However, these serious adverse events fully resolved, and the patients achieved neutrophil engraftment on day 56. All other patients achieved neutrophil engraftment within 43 days of the exa-cell infusion.
No deaths, discontinuations, or malignancies were reported.
António Almeida, MD, who was not involved in the research, said the findings suggest an important and potentially safer alternative to conventional bone marrow transplantation.
"What they're doing here is eliminating the patients' bone marrow but then giving them back their own cells, except they’ve been edited to produce hemoglobin normally," said Almeida, of the Hospital da Luz, in Lisbon, Portugal, and EHA president-elect. "This means we eliminate a lot of the issues that we have with transplantation, in terms of the donor bone marrow attacking the recipients, such as graft versus host disease or problems with immunosuppression."
Almeida added: "It also means that the engraftment rate is much higher because we are just fixing their own bone marrow and giving it back, which is really important, so I think this is very novel and exciting."
The CLIMB THAL-111 and CLIMB SCD-121 trials were sponsored by Vertex Pharmaceuticals Inc. Locatelli is on the advisory board for Vertex Pharmaceuticals. Almeida reported no relevant disclosures.
The 2022 European Hematology Association Annual Meeting. Abstract LB2367. Presented June 12, 2022.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Credits:
Lead image: Stocktrek Images/Getty Images
Medscape Medical News © 2022
Cite this: New Therapy May Offer 'Functional Cure' for Two Blood Disorders - Medscape - Jun 14, 2022.









Comments